Harbottle GP clinic proposal
Northumbria Healthcare NHS Foundation Trust has written to all patients of The Rothbury Practice with the following information.
If you need the following information in an alternative format, please email nencicb-nor.rothburypractice@nhs.net.
A GP or nurse from The Rothbury Practice, which is part of Northumbria Primary Care, currently provides a clinic, once a week on a Thursday, in the village hall in Harbottle.
This clinic has been in place since 2009. In 2015 the previous provider (GP) decided to end their GP contract and the GP service in Harbottle faced closure. Following the community response, clinicians from The Rothbury Practice have provided GP patient care in the village.
Northumbria Primary Care is working with the North East and North Cumbria Integrated Care Board to consider how we can potentially enhance healthcare services in rural Northumberland. We need to ensure that what we do is sustainable, both financially and in terms of workforce.
What is being proposed
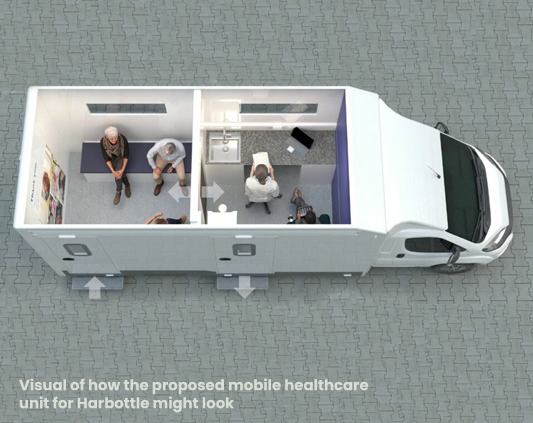
The proposal being considered is moving the GP/nurse clinic, that is currently provided from Harbottle Village Hall, into a mobile healthcare unit. The mobile healthcare unit would be the permanent location from which the Harbottle weekly GP/nurse clinic would be delivered.
We would like to assure people that this proposal would not result in a reduction to current primary care services provided in Harbottle.
Patient benefits
The additional benefit of services being delivered from a mobile unit is that it would be able to travel and deliver primary (GP), public health and community/voluntary sector services in this rural area of Northumberland on the days that it is not in Harbottle. Examples of the services that could be delivered in local communities include vaccination clinics, annual health checks, blood pressure checks, public health services (like stop smoking clinics) and voluntary and community sector engagement and services.
With the unit being mobile, where possible, it could be responsive to the healthcare needs of local communities, as long as the workforce is available to support this.
We are also in the very early stages of exploring if the community team at Northumbria Healthcare NHS Foundation Trust could use the mobile healthcare unit to potentially offer appropriate services closer to home.
The cost of operating a mobile healthcare unit would be similar to providing GP services from the village hall in Harbottle. As a result, this option would be financially sustainable with the potential to offer additional services to local communities in Northumberland.
Details about the mobile healthcare unit
The mobile healthcare unit would be a clinical environment, comfortable, heated and wheelchair accessible. It would also have separate waiting and consulting rooms to enable patient privacy. Where the mobile healthcare unit would park in Harbottle and where people would access a toilet are things that are currently under discussion. It would be driven by staff who have a valid UK driving licence and training. We acknowledge that the winter weather in Northumberland is also an important consideration. Planning and regular maintenance would help ensure, as much as possible, that the vehicle would be where it needs to be.
Getting feedback is crucial to help inform and shape this proposal
We would like as many patients, members of the public and stakeholders as possible to help inform if a mobile healthcare unit could be a viable option and if so, how it could be used to deliver GP, public health and community/voluntary services. This proposal is in the early stages of being developed and we know that we must ensure that the use of a mobile unit could be sustainably managed and that there is a community need for what it could be used for.
You can tell us your views in a few different ways – we welcome feedback from all
Patients registered with The Rothbury Practice (regardless of which surgery they access care from) will receive either a hard copy of or text message with a website link to a letter, survey, and a frequently asked questions (FAQs) document.
- You can complete this online survey
- You can complete a hard copy survey – these will be available from and will need to be dropped off at the weekly Harbottle clinic on a Thursday morning or The Rothbury Practice or Longframlington surgery receptions.
All surveys need to be completed by Friday 23 February 2024.
- If you have a planned appointment at the clinic in Harbottle on Thursday 14 December or Thursday 1 February 2024, you will be able to speak to someone if you would like to give feedback.
- If you have a planned appointment at The Rothbury Practice on Tuesday 19 December or Thursday 18 January 2024 between 10.00am and 2.00pm you will be able to speak to someone if you would like to give feedback.
- You can attend a drop-in engagement session for patients and stakeholders – they will be held on Tuesday 9 January 2024 between 10.00am and 2.00pm and Tuesday 13 February between 3.00pm and 7.00pm at Harbottle Village Hall, Harbottle, NE65 7DG. You do not need to register to attend. All are welcome to attend.
- You can also write to or email the practice management team – The Rothbury Practice, Whitton Bank Road, Rothbury, Northumberland, NE65 7RW or encicb-nor.rothburypractice@nhs.net.
- If you would like to give feedback to someone independent, please contact Healthwatch Northumberland.
Next steps and time-line
This option has been approved in principle by the North East and North Cumbria Integrated Care Board, subject to engagement with the community and stakeholders. Following the programme of engagement with patients and a wide range of stakeholders, all feedback will be considered, and a final decision will be made, hopefully in March next year. The earliest a mobile healthcare unit could be put in place is May 2024.