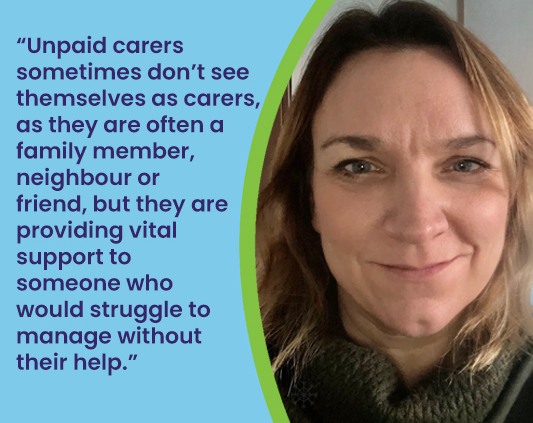
Debra Blakey is the Chief Executive Officer of Carers Northumberland and one of our organisational board members. Debra has been on the board for six years, providing invaluable experience and insight. Debra spoke to us about the work of Carers Northumberland and the important relationship with Healthwatch Northumberland.
Debra says “Carers Northumberland is a charity that aims to improve the lives of unpaid carers in the county. We support unpaid carers of all ages, including adult carers of adults, young carers (aged under 18 years) and parent carers (caring for someone who is under 18 years with additional needs). Unpaid carers sometimes don’t see themselves as carers, as they are often a husband, wife, mother, father, brother, sister, neighbour, or friend, but they are providing vital support to someone who would struggle to manage without their help.
We offer advice, information and support to our 7000+ registered carers. We do this in a variety of ways, including via our telephone information line, carer groups, workshops and training, benefits and financial support, grants to enable carers to take a break from caring, support to navigate social care and health provision, plus trips, events, and activities.
I have worked for Carers Northumberland since 2008 (almost as long as it’s been going!) when I joined as an Administration Officer, and I’ve been in the role of Chief Executive Officer since 2018. I have a degree in Criminology and worked in both private organisations and for Northumbria Police before starting in the voluntary sector at Carers Northumberland. I am passionate about making a difference to people’s lives and having worked for a charity for over 15 years I couldn’t see myself working in any other type of organisation now.
I enjoy reading, going out to eat, and love visiting new places. I’m also a keen runner (well I run so that I can enjoy eating cake) and I believe in the benefits of exercise for mental wellbeing. I actually think I enjoy how good I feel about myself after a run more than the actual run itself.
Probably the achievement I am most proud of is securing funding to pilot a Young Carer Support Service to run alongside our existing service for adult carers. We launched the service in 2020 during a global pandemic, but it has gone from strength to strength, and we are now working very closely with schools in the county to raise awareness of young carers in education to encourage early identification and provide tailored support.
Carers Northumberland has been an organisational board member of Healthwatch Northumberland since its inception, which highlights how valuable our relationship is. Both organisations are striving to improve the health and social care landscape for service users, patients and their families and carers and we have collaborated on several major pieces of work over the past ten years. Being able to feed the views of carers into Healthwatch Northumberland ensures that the carer voice is heard by key decision-makers in the county is invaluable.“
Carers Northumberland supports all carers of all ages and can be contacted by telephone: 01670 320025, email: info@carersnorthumberland.org.uk or visit the website.